In a time when many hospitals across Saskatchewan are regularly bursting at the seams with patients and there are chronic health-care staffing shortages, one health centre in southeastern Saskatchewan has the opposite problem: they have the doctors, the nurses, and the necessary support to treat patients, but in many cases can’t do so.
According to the SHA website, the Galloway Health Centre in Oxbow has a “robust ER, eight temporary care beds, and 12 long term care beds.”
It also boasts a laboratory and X-ray facility, and offers palliative care, recreational therapy, and respite care. There are at least three physicians for a local population of about 1,200, a variety of nurses, and other health-care workers staffing the facility.
Read more:
- Health-care costs will rise significantly as population ages: Report
- Sask. offering new incentives for high-demand medical residents
- Health-care cuts forced woman to give birth on side of highway: Sask. NDP
However, according to families, a former healthcare worker, Oxbow’s mayor Doug Pierce and the RM of Enniskillen chief administrative officer Pamela Bartlett, if someone has a respiratory illness, broken bones or even a heart attack that would necessitate a brief hospital stay, they can’t be treated for more than 24 hours at the fully staffed health centre.
According to provincial rules, the patient must be sent to a facility where beds are allowed for acute care use, at least an hour away.
Many who live in the area say the facility isn’t operating to its full capability. Patients are being sent to Estevan, Arcola, Regina, and even across the province to Swift Current, unnecessarily.
Bartlett said there’s a lot of frustration from residents and health-care workers alike.
“Somebody can stay there for 24 hours under observation. After that, they have to be transferred out to a hospital unless there is palliative care, convalescent care,” she said.
“If they have to be transferred to Estevan or Arcola, not only are we mismanaging the use of doctors, but we’re mismanaging the use of ambulances because if they are on any medications, IVs, then chances are they’re going to have to be transferred by ambulance,” she said.
Bartlet said families also then have to find alternate arrangements to visit their loved ones, who also feel displaced.
“Not only that, you have the patient who is used to the doctors in this area as well as the nursing staff. They also now have to be transferred out of their own community and it can be quite stressful on the patient and the family for something they should be able to stay in our community for,” she added.
She wrote a letter in August to the provincial government, expressing the collective frustration.
“Please, please, we can not ask enough to escalate this situation so that we can have AT LEAST 2 acute beds. From what I understand, the only difference between Oxbow and Arcola (northwest of Oxbow) is that Arcola can run a few more labs. If equipment is needed, please let us know what is needed. We are asking for openness, transparency and urgency in this situation,” she wrote.
Pierce also said in a telephone call that concerns about the lack of acute care beds have been brought to council.
Frustrated families
Former Galloway Centre R.N. Donna Cooney said two weeks ago her elderly mother-in-law went there looking for help after suffering from a respiratory infection. Instead of being treated at the health centre, she was told by her doctor that she would need to be transferred to another location.
“Estevan (hospital) did not have placement to take her; she would go to Arcola,” she recalled.
Cooney said their physician in Arcola questioned why her mother-in-law could not be treated in Oxbow.
“He threw up his hands and said ‘yes, I know. I understand the situation.’”
In another case several months ago, Oxbow resident Jim Brock’s aunt fell out of her bed at a long-term care facility. An ambulance was called, and because there were no acute care beds in Oxbow, she was taken to Estevan.
“There’s no beds open there. They took her to Moose Jaw, transferred ambulances and took her to Swift Current, five hours from here.” he said.
“She was there for two days and they sent her back to Estevan overnight, and then sent her back here…by the time she got back from Estevan she was crying and depressed and says ‘I’m finished. I’m gonna die.’”
Brock’s aunt has since fallen out of her bed again, but remained on the floor out of fear she would again be taken for treatment hours from home.
“She’s afraid to call anybody and let them know because it might be the same experience again,” he said.
For Shelley Gunderman’s husband, the problems began after he had hip replacement surgery in Regina last summer but became extremely ill in the days after.
“He got sicker and sicker, so I brought him to the Galloway Health Centre and we saw Dr.(Nic) Botha, who was awesome. They did some tests… and decided to send him to Estevan for an ultrasound,” she recalled.
When in Estevan, the couple was told they could not go back to Oxbow for antibiotic treatment. Gunderman said Botha had been advocating for her her husband to come back. She said health-care staff in Estevan also questioned that.
“Why is he here? Why can’t he go back to Oxbow? I don’t understand why we have to treat him here,” she recalled.
Since that time, Gunderman and her husband travel to Estevan for treatment.
“Our doctors are frustrated, our nurses are frustrated, because they can not offer the care that they know they can provide,” she said.
Health ministry response
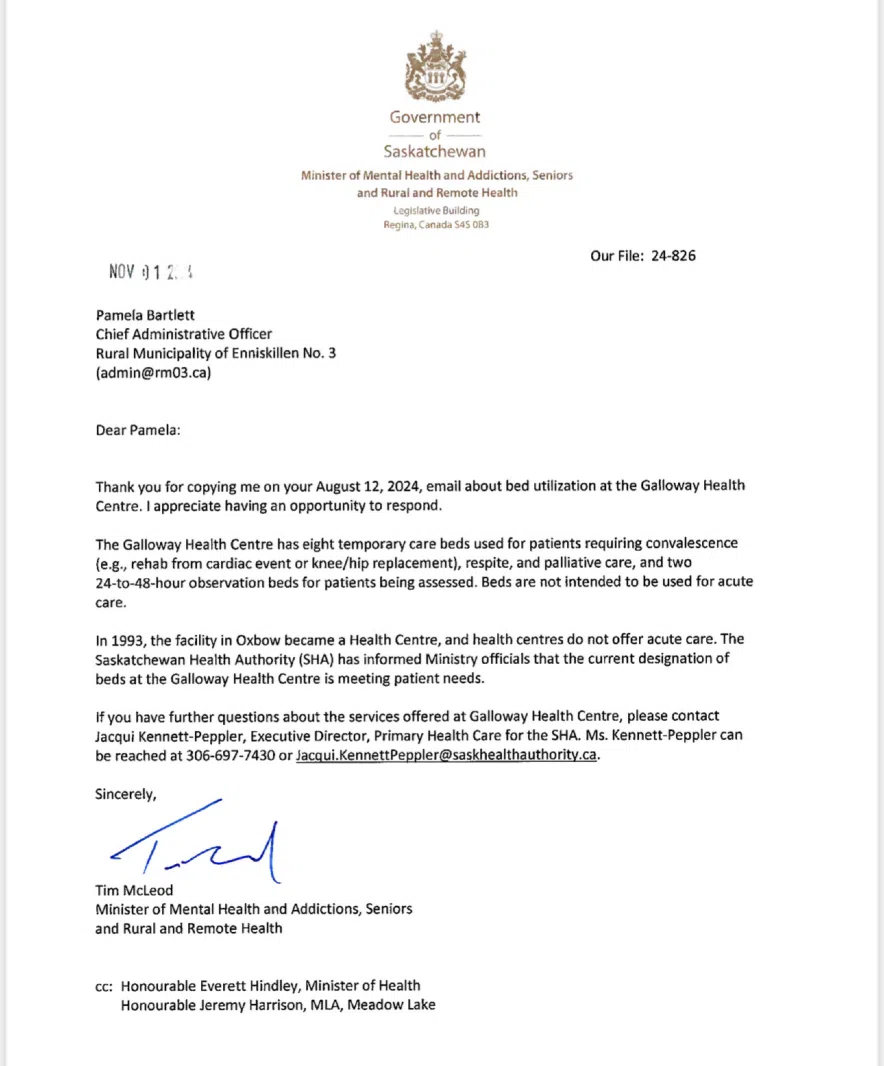
According to a letter written to Bartlett from former rural and remote health minister Tim McLeod dated November 2024, in 1993 the Oxbow facility became a health centre, and health centres “do not offer acute care.”
McLeod also wrote, “the Saskatchewan Health Authority (SHA) has informed the ministry that the current designation of beds is meeting patient needs.”
According to Bartlett, that is just not the case.
“We have our doctors, we have our nurses. They deserve to be able to take care of patients. Our community deserves to be taken care of by our doctors and nurses,” she said.
Brock also said he doesn’t understand the former health minister’s thinking.
“Give them (Galloway Centre) some acute care beds back so the doctors can do their job. The doctors’ hands are tied here. It’s like having a clinic here and that’s all. If you have anything more than that you have to be prepared (for) somebody to drive you or get in an ambulance and go someplace else,” he said.
650 CKOM/980 CJME requested an interview with the new rural and remote health minister, Lori Carr multiple times over several days.
Instead, a statement sent from the ministry said ensuring Oxbow and area residents get reliable and consistent access to health care is a priority, but that did not mean including access to acute care beds.
“While we are not actively considering redesignation of the Galloway Health Centre, we are committed to working with the community and the Saskatchewan Health Authority on maintaining stable physician and staffing in Oxbow.”
Read more:
- Health-care costs will rise significantly as population ages: Report
- Sask. offering new incentives for high-demand medical residents
- Health-care cuts forced woman to give birth on side of highway: Sask. NDP
It’s not clear, why that decision is not being reconsidered.
An attempt was also made to reach out to Doctor Nic Botha at the Galloway Health Centre, however he is currently out of the country.
Editor’s Note: This story has been updated to correct a misspelling of Gunderman’s name.